Ultrasound-guided cannulation of the internal jugular vein uses real-time (dynamic) ultrasound to guide venipuncture and a guidewire (Seldinger technique) to thread a central venous catheter through the internal jugular vein and into the superior vena cava. Three approaches (central, anterior, and posterior) are used; the central approach is described here.
Ultrasound guidance for placement of internal jugular lines increases the likelihood of successful cannulation and reduces the risk of complications. When ultrasound guidance and trained personnel are available, this method of placement is preferred.
An internal jugular central venous catheter (CVC) or a peripherally inserted central catheter (PICC) is usually preferred to a subclavian CVC (which has a higher risk of bleeding and pneumothorax) or a femoral CVC (which has a higher risk of infection).
(See also Vascular Access, Central Venous Catheterization, and How To Do Internal Jugular Vein Cannulation.)
Indications for Internal Jugular Vein Cannulation, US-Guided
Secure or long-term venous access that is not available using other sites
Inability to obtain peripheral venous access or intraosseous infusion
IV infusion of fluids and medications for patients in cardiac arrest
IV infusion of medications that may be irritating to veins when administered peripherally (eg, high-concentration fluids, chemotherapy, vasopressors, parenteral nutrition)
IV infusion of high flows or large fluid volumes beyond what is possible using peripheral venous catheters
Hemodynamic monitoring (eg, central venous pressure, central venous oxyhemoglobin saturation, cardiac pressures via pulmonary artery catheters)
Hemodialysis or plasmapheresis
Transvenous cardiac pacing or pulmonary arterial monitoring (Swan-Ganz catheter)*
Placement of inferior vena cava filter
* For transvenous cardiac pacing or pulmonary arterial monitoring, a right internal jugular or a left subclavian cannulation typically is preferred.
Contraindications to Internal Jugular Vein Cannulation, US-Guided
Absolute contraindications
Untrained or inexperienced ultrasound operator
Unsuitable internal jugular vein, thrombosed (incompressible) or inaccessible as seen by ultrasound
Local infection at the insertion site
Antibiotic-impregnated catheter in a patient with an allergy to the specific antibiotic
Relative contraindications
Coagulopathy, including thrombocytopenia or anticoagulant medications (including antiplatelet medications)*
Local anatomic distortion, traumatic or congenital, or gross obesity
Malignant superior vena cava syndrome
Severe cardiorespiratory insufficiency or increased intracranial or intraocular pressure (patients will be compromised by Trendelenburg [head down] positioning)
History of prior catheterization of the internal jugular vein (prior catheterization may have resulted in scar tissue formation making catheter placement more difficult)
Uncooperative patient (should be sedated if necessary)
Left bundle branch block (a guidewire or catheter in the right ventricle can induce complete heart block)
* Anticoagulant medications (eg, for atrial fibrillation) increase the risk of bleeding with internal jugular cannulation, but this risk must be balanced against the increased risk of thrombosis (eg, stroke) if anticoagulation is reversed. Discuss any contemplated reversal with the clinician managing the patient's anticoagulation and then with the patient. A femoral line may be preferred.
Complications of Internal Jugular Vein Cannulation, US-Guided
(See also Complications of central venous catheterization.)
Potential complications include
Arterial puncture
Hematoma
Pneumothorax
Damage to the vein
Hemothorax
Air embolism
Catheter misplacement*
Arrhythmias or atrial perforation, typically caused by guidewire or catheter
Nerve damage
Infection
Thrombosis
* Rare complications due to catheter misplacement include arterial catheterization, hydrothorax, hydromediastinum, and damage to the tricuspid valve.
Guidewire or catheter embolism also rarely occurs.
To reduce the risk of venous thrombosis and central line-associated bloodstream infection (CLABSI), CVCs should be removed as soon as they are no longer needed.
Equipment for Internal Jugular Vein Cannulation, US-Guided
Sterile procedure, barrier protection
Antiseptic solution (eg, chlorhexidine-alcohol, chlorhexidine, povidone-odine, alcohol)Antiseptic solution (eg, chlorhexidine-alcohol, chlorhexidine, povidone-odine, alcohol)
Large sterile drapes, towels
Sterile hats, masks, gowns, gloves
Face shields
Ultrasound guidance
Ultrasound machine with a high-frequency (eg, 5 to 10 MHz), linear array probe (transducer)
Ultrasound gel, nonsterile and sterile
Sterile probe cover to ensheathe probe and probe cord, sterile rubber bands (alternatively, the probe may be placed within a sterile glove and the cord wrapped within a sterile drape)
Seldinger (catheter-over-guidewire) technique
Cardiac monitor
Local anesthetic (eg, 1% lidocaine without epinephrine, approximately 5 mL)Local anesthetic (eg, 1% lidocaine without epinephrine, approximately 5 mL)
Small anesthetic needle (eg, 25 to 27 gauge, 3 cm [approximately 1 inch] long)
Large anesthetic/finder* needle (22 gauge, 4 cm [approximately 1.5 inches] long)
Introducer needle (eg, thin-walled, 18 or 16 gauge, with internally beveled hub, 6 cm [approximately 2.5 inches] long)
3- and 5-mL syringes (use slip-tip syringes for the finder and introducer needles)
Guidewire, J-tipped
Scalpel (#11 blade)
Dilator
Central venous catheter (adult: 8 French or larger, minimum length for internal jugular catheter is 15 cm [approximately 6 inches] for right side, 20 cm [approximately 8 inches] for left side)
Sterile gauze (eg, 10 × 10 cm [4 × 4 inch] squares)
Sterile saline for flushing catheter port or ports
Nonabsorbable nylon or silk suture (eg, 3-0 or 4-0)
Chlorhexidine patch, transparent occlusive dressingChlorhexidine patch, transparent occlusive dressing
* A finder needle is a thinner needle used for locating the vein before inserting the introducer needle. It is usually not needed for ultrasound-guided cannulations.
The external diameter of the CVC should be less than or equal to one-third of the internal diameter of the vein (as measured by ultrasound) to reduce the risk of thrombosis.
Having 1 or 2 assistants is helpful.
Additional Considerations for Internal Jugular Vein Cannulation, US-Guided
The short-axis (cross-sectional, transverse) ultrasound view is easy to obtain and is the better view for identifying veins and arteries and their orientation to each other. Identifying a needle tip in cross section requires some skill, because the needle appears as an echogenic (ie, white) dot and the tip can be distinguished only by the dot's disappearance and reappearance as the needle tip traverses back and forth across the imaging plane. The short-axis view typically is used to determine a suitable venous impalement site and to guide steeply angled (eg, ≥ 45°) needle insertions.
The long-axis (longitudinal, in-plane) ultrasound view is technically more difficult to obtain (must keep probe, vein, and needle in one plane), but it shows the needle longitudinally, so the entire needle—including the tip—can be imaged continuously as it approaches and enters the vein; this continuous view helps avoid aberrant placement. The long-axis view is helpful when the angle of needle insertion is shallow (eg, in axillary/subclavian cannulations) and to affirm proper longitudinal needle alignment during short-axis insertions.
Cannulation attempts sometimes fail. Do not exceed 2 or 3 attempts (which increases the risk of complications), and use new equipment with each attempt (ie, do not re-use needles, catheters, or other equipment because they may have become blocked with tissue or blood).
During cardiopulmonary arrest, or even low blood pressure and hypoxia, arterial blood may be dark and not pulsatile and may be mistaken for venous blood.
If the carotid artery is errantly cannulated by either the tissue dilator or the CVC, leave the dilator or catheter in place and obtain surgical consultation for possible surgical removal.
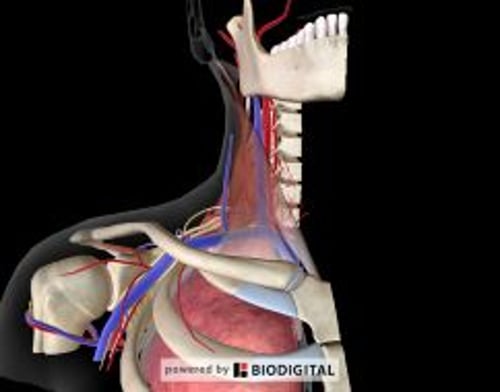
Relevant Anatomy for Internal Jugular Vein Cannulation, US-Guided
The anterior cervical triangle is bordered by the clavicle inferiorly and by the sternal and clavicular heads of the sternocleidomastoid muscle medially and laterally.
Within the anterior cervical triangle, the internal jugular vein usually lies superficial and lateral (often minimally lateral) to the carotid artery; however, because variant orientation of these vessels occurs regularly (in 9 to 19% of patients), ultrasound guidance is particularly helpful in internal jugular vein cannulation.
Most commonly, the central approach to the internal jugular vein is used. An introducer needle is inserted into the skin inside the apex (superior angle) of the triangle and is advanced proximally (caudally) at approximately a 45° angle to the skin to intersect the vein.
The skin insertion site is influenced by both the imaging and the dimensions of the transducer tip (ie, the skin insertion site for long-axis ultrasound guidance may be several centimeters distal to that for short-axis ultrasound guidance).
The right internal jugular vein is usually preferred over the left for cannulation because it has a larger diameter and affords a straighter path to the superior vena cava.
Positioning for Internal Jugular Vein Cannulation, US-Guided
Raise the bed to a comfortable height for you (ie, so you may stand straight while doing the procedure).
Place the patient supine or in Trendelenburg position (bed tilted with the head down 15 to 20°) to distend the internal jugular vein and prevent air embolism.
Turn the patient's head slightly to the contralateral side to preliminarily expose the internal jugular vein but not cause overlap with the carotid artery (during the procedure, you will use ultrasound to optimally expose the vein).
Stand at the head of the bed.
Step-by-Step Description of Internal Jugular Vein Cannulation, US-Guided
Preliminary preparation (nonsterile)
Check that the ultrasound machine is configured and functioning correctly: Ensure that the screen image you are seeing correlates to the spatial orientation of the probe as you are holding and moving it. The side mark on the probe tip corresponds to the marker dot on the ultrasound screen. Adjust the screen settings and probe position if needed to attain an accurate left-right orientation.
Do a nonsterile ultrasound inspection (ie, using an uncovered probe and nonsterile gel) and determine whether the vein is suitable for cannulation. Use a short-axis (cross-sectional) view. Begin at the apex of the anterior cervical triangle, and slowly slide the probe proximally (toward the clavicle) along the lateral border of the sternal head of the sternocleidomastoid. Blood vessels are hypoechoic (appear black on the ultrasound screen). Veins are generally larger, thin-walled, and ovoid (rather than thick-walled and round) and are more easily compressed (by gentle pressure on overlying skin) than their paired arteries. The size of the internal jugular vein varies with respiration and is increased by the Trendelenburg position and the Valsalva maneuver.
Venous thrombosis may appear as an echogenicity (gray irregularity) in the lumen but often is diagnosed because the thrombosed vein is incompressible. Thrombosis disqualifies the vein as a suitable cannulation site.
Cannulate a central vein at a site of optimal short-axis imaging (ie, large-diameter cross section of the vein, with no overlying artery).
Attach the cardiac monitor to the patient and turn it on.
Prepare the equipment
Place sterile equipment on sterilely covered equipment trays.
Use appropriate personal protective equipment.
Draw the local anesthetic into a syringe.
Attach the introducer needle to a 5-mL syringe with 1 to 2 mL of sterile saline in it. Align the bevel of the needle with the volume markings on the syringe.
Pre-flush all lines of the CVC with 3 to 5 mL of sterile saline and then close the ports with caps or syringes.
When flushing a central line, use a 10-mL syringe (or one of equal or greater diameter) and do not push too hard to avoid rupturing the line.
Prepare the sterile field
Swab a broad area of skin with antiseptic solution, encompassing the side of the neck, clavicle, and anterior chest to below the ipsilateral nipple. Creating this broad sterile area permits immediately switching to subclavian vein cannulation or unassisted (“blind”) internal jugular cannulation should the ultrasound-guided jugular cannulation attempt fail.
Allow the antiseptic solution to dry for at least 1 minute.
Place sterile towels around the site.
Place large sterile drapes (eg, a full-body drape) to establish a large sterile field.
Put on sterile mask and hat.
Put on sterile gown and gloves.
Place a sterile cover over the ultrasound probe
Direct your assistant (nonsterile) to coat the probe tip with nonsterile ultrasound gel and then hold the probe, with the tip pointing up, just outside the sterile field.
Insert your gloved dominant hand into the sterile probe cover.
Grasp the tip of the probe with your dominant hand (now covered by the probe cover).
Use your gloved nondominant hand to unroll the sterile cover over the probe and completely down the cord. Do not touch the uncovered cord nor allow it to touch the sterile field as you unroll the cover.
Pull the cover tightly over the probe tip to eliminate all air bubbles.
Wrap sterile rubber bands around the probe to secure the cover in place, ensuring the nonsterile gel covers the tip of the probe.
The covered probe may now rest on the sterile drapes.
Anesthetize the cannulation site
Apply sterile ultrasound gel to the covered probe tip.
Use short-axis ultrasound guidance:
Attain an optimal cross-sectional image of the internal jugular vein (near the apex of the anterior cervical triangle, if possible). Press lightly with the probe tip to avoid distorting the image size and shape of the vein.
Slide the probe transversely as needed to place the imaged vein at the center of the ultrasound screen. When the vein is centered on the ultrasound screen, the midpoint of the probe becomes a surface marker designating the luminal center of the underlying vein.
Keep the probe in this spot.
On the ultrasound screen, measure the depth to the center of the vein. When using short-axis ultrasound guidance, insert procedural needles (local anesthetic and introducer needles) into the skin at a point distal and perpendicular to the midpoint of the probe by the same distance as the vein depth. Then, initially advance the needle into the skin at a 45° angle directed toward the midpoint of the probe. Keep gentle negative pressure on the syringe plunger as you advance.
Place a wheal of anesthetic at the needle entry point and then inject anesthetic into the skin and soft tissues along the 45° path leading toward the vein.
Slightly tilt the probe along the long axis of the vein as you advance the anesthetic needle to continually identify the needle tip and keep it safely distant from the vein and artery.
Insert the introducer needle
Continue to use short-axis ultrasound guidance (as described above for the local anesthetic injection).
Insert the introducer needle.
Maintain ultrasound visualization of the needle tip as you advance by continually tilting the probe slightly along the long axis of the vein (the needle tip appears and disappears as the ultrasound plane sweeps back and forth over it).
If the needle tip strays from the vein, adjust the lateral direction of the needle to keep the needle tip above the center of the vein. If the needle tip is approaching the vein too slowly, withdraw the needle a bit, increase the angle of insertion, and re-advance.
As the needle tip approaches the vein, temper your speed and angle of insertion so the needle enters with as much control as possible. The superficial wall of the vein will indent when the needle tip encounters it. The needle then pops through the wall to enter the lumen, accompanied by a flash of dark red blood in the barrel of the syringe.
Hold the syringe motionless in this spot and visualize the tip of the needle at all times. Displacement is common, and even a slight movement may displace the needle tip from the vein.
Optional: If the accessible vein segment is long enough to accommodate the long axis of the probe, you may prefer to use the short-axis (cross-section) view first to aim the needle at the vein, and then rotate the probe 90° to attain the long-axis (in-plane, longitudinal) view of the needle and vein, which provides better imaging of the venipuncture. Move the probe as needed to keep both the needle and the vein in sight (in-plane). Press lightly with the probe tip so the vein remains under the tip and does not roll to the side.
Assess the blood return
Continue to hold the syringe motionless.
Securely grasp the needle hub and also hold it motionless.
Remove the syringe from the needle hub and briefly let blood flow out to confirm that the blood is venous (ie, dark red and flowing, but not pulsatile). Then immediately cover the hub with your thumb to stop the blood flow and prevent air embolism.
However, if the blood is bright red and pulsatile (arterial), terminate the procedure. Remove the needle and use gauze squares for 10 minutes to hold external pressure on the area and to help prevent bleeding and hematoma.
Insert the guidewire
Carefully rotate the introducer syringe such that the bevel of the needle now faces medially (ie, toward the heart and away from the subclavian vein).
Insert the J-curved end of the guidewire into the introducer needle, with the J curve facing medially (ie, in the same direction as the needle bevel).
Advance the guidewire through the needle and into the vein. You may use ultrasound guidance (either short- or long-axis) to verify the guidewire entering the vein. Do not force the wire; it should slide smoothly. Advance the wire 10 to 15 cm for a right-sided internal jugular insertion, 15 to 20 cm for a left-sided insertion, or until ectopic heartbeats occur (withdraw from this point until ectopy stops).
If you feel any resistance as you advance the guidewire, stop advancing it. Try to gently withdraw the wire slightly, rotate it slightly, and then re-advance it, or try to gently withdraw the wire entirely, reestablish the needle tip within the vein (confirmed by venous blood return), and then reinsert the wire.
However, if you feel any resistance as you withdraw the guidewire, terminate the procedure and withdraw the needle and guidewire together as a unit (to prevent the needle tip from shearing through the guidewire within the patient). Then use gauze squares for 10 minutes to hold external pressure on the area and to help prevent bleeding and hematoma.
Once the guidewire has been inserted, continue to hold it securely in place with one hand and maintain control of it throughout the remainder of the procedure to avoid wire embolism.
Remove the introducer needle (after successful guidewire insertion)
First, securely hold the guidewire distal to the needle and pull the needle from the skin.
Then, securely hold the guidewire at the skin surface and slide the needle down the remaining length of the guidewire to remove the needle.
Widen the insertion tract
Extend the skin insertion site: Using the scalpel, make a small stab incision (approximately 4 mm) into the skin insertion site, avoiding contact with the guidewire, to enlarge the site and allow it to accommodate the larger diameters of the tissue dilator and the catheter.
Advance the tissue dilator over the guidewire: First, grasp the guidewire at the skin and slide the dilator down the length of the wire to the skin. Then grasp the wire just distal to the dilator, hold the dilator near the skin surface, and use a corkscrew motion as needed to stepwise insert dilator to pass through the wall of the vein. Maintain your grasp on the wire at all times during the insertion.
Remove the dilator: First, securely hold the guidewire distal to the dilator and pull the dilator from the skin. When the guidewire is visible at the skin surface, completely remove the dilator by sliding it down the remaining length of the guidewire.
Maintain your grasp on the guidewire at the skin surface.
Place the catheter
Advance the catheter over the guidewire to the skin surface: Hold the guidewire fixed at the skin surface, thread the catheter tip over the distal end of the guidewire, and slide the catheter down to the skin surface at a 45° angle. The distal end of the guidewire should now be protruding from the port hub.
If the distal end of the guidewire is not protruding from the port hub, incrementally advance the guidewire outward from the skin surface while holding the catheter tip close to the surface until the guidewire protrudes.
Continue to advance the catheter into the vein: Grasp and control the guidewire where it protrudes from the hub. Hold the catheter near its tip and insert the tip through the skin. Then, in increments of several centimeters and using a corkscrew motion as necessary, stepwise advance the entire length of the internal jugular catheter. If ectopic heartbeats occur, slowly withdraw the catheter until ectopy stops.
Use ultrasound to verify intravenous placement of the catheter.
Maintain your grasp on both the guidewire and the catheter.
Remove the guidewire: Withdraw the guidewire while holding the catheter securely in place at the skin surface.
Flush each catheter port with saline: First, draw any air from the line and confirm venous blood flow into the hub. Then, using a 10-mL syringe (or one of equal or greater diameter) and without using excessive force, push 20 mL of saline into the line to clear it.
Dress the site
If the patient is awake or minimally sedated, use 1% lidocaine to anesthetize the skin at the planned suture locations.If the patient is awake or minimally sedated, use 1% lidocaine to anesthetize the skin at the planned suture locations.
Place a chlorhexidine-impregnated disk on the skin at the catheter insertion point. Place a chlorhexidine-impregnated disk on the skin at the catheter insertion point.
Suture the skin to the mounting clip on the catheter.
To prevent pulling on the insertion site, suture the catheter at a second site so that a curved or looped segment of catheter lies between the two sites.
Apply a sterile occlusive dressing. Transparent membrane dressings are commonly used.
Aftercare for Internal Jugular Vein Cannulation, US-Guided
Prior to using the catheter, do chest radiography to confirm that the tip of a jugular (or subclavian) venous catheter lies in the superior vena cava near its junction with the right atrium (the catheter can be advanced or retracted if not in the appropriate position) and to confirm that pneumothorax has not occurred.
The red arrow points to the tip of a left subclavian venous port catheter (placed appropriately in the lower superior vena cava).
Warnings and Common Errors for Internal Jugular Vein Cannulation, US-Guided
The tip of a CVC must never lie in the right atrium because the atrium is thin-walled and easily perforated.
Cardiac ectopy may be induced by a guidewire or catheter in the right atrium or ventricle.
Never lose grasp of the guidewire.
During cardiopulmonary arrest, or even low blood pressure and hypoxia, arterial blood may be dark and not pulsatile and may be mistaken for venous blood.
To help prevent air embolism, CVCs should be inserted (and removed) with the vascular cannulation site positioned dependant to the heart.
Drugs Mentioned In This Article