The liver is a metabolically complex organ. Hepatocytes (liver parenchymal cells) perform the liver’s metabolic functions:
Formation and excretion of bile as a component of bilirubin metabolism (see Overview of bilirubin metabolism)
Control of cholesterol metabolism
Formation of urea, serum albumin, clotting factors, enzymes, and numerous other proteins
Metabolism or detoxification of medications and other foreign substances
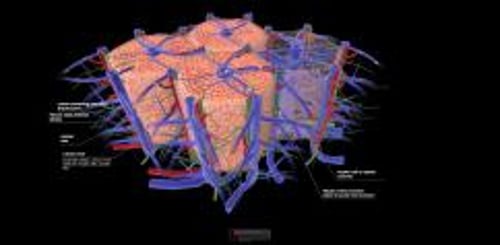
Overview of liver structure
At the cellular level, hepatocytes are organized within a lobule, which is a hexagonally shaped groups of cells with a hepatic vein at the center, and portal triads around the periphery. The portal triads consist of adjacent and parallel terminal branches of bile ducts, portal veins, and hepatic arteries. Blood flows from the hepatic artery and portal vein (in the portal triads) in the periphery, through the sinusoids between the hepatocytes, toward the central vein. Consequently, hepatocytes at the center of the lobule are most susceptible to ischemia because oxygen and nutrients have been extracted by hepatocytes as blood flows through the sinusoids from the periphery. Smaller channels, called bile canaliculi, drain bile secreted by the hepatocytes into the intrahepatic bile ducts at the periphery.
Copyright © 2023 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
Image courtesy of Danielle Tholey, MD, and M. Isabel Fiel, MD, MS, FAASLD.
Overview of bilirubin metabolism
The breakdown of hemoglobin produces bilirubin (an insoluble waste product) and other bile pigments. Bilirubin must be made water soluble to be excreted. This transformation occurs in 5 steps: formation, plasma transport, liver uptake, conjugation, and biliary excretion.
Formation: Approximately 250 to 350 mg of unconjugated bilirubin forms daily; 70 to 80% derives from the breakdown of degenerating red blood cells, and 20 to 30% (early-labeled bilirubin) derives primarily from other heme proteins in the bone marrow and liver. Hemoglobin is degraded to iron and biliverdin, which is converted to bilirubin.
Plasma transport: Unconjugated (or "indirect") bilirubin is not water soluble and so is transported in the plasma bound to albumin. It cannot pass through the glomerular membrane into the urine. Albumin binding weakens under certain conditions (eg, acidosis), and some substances (eg, salicylates, certain antibiotics) compete for the binding sites.
Liver uptake: The liver takes up bilirubin rapidly but does not take up the attached serum albumin.
Conjugation: Unconjugated bilirubin in the liver is conjugated to form mainly bilirubin diglucuronide (conjugated [or "direct"] bilirubin). This reaction, catalyzed by the microsomal enzyme glucuronyl transferase, renders the bilirubin water soluble.
Biliary excretion: Conjugated bilirubin, together with other bile constituents, is secreted into tiny bile canaliculi. These canaliculi, formed by adjacent hepatocytes, progressively coalesce into ductules, interlobular bile ducts, and larger hepatic ducts into the hepatic duct. The main hepatic duct joins the cystic duct from the gallbladder to form the common bile duct, which drains into the duodenum at the ampulla of Vater.
In the intestine, bacteria metabolize bilirubin to form urobilinogen, much of which is further metabolized to stercobilins, which render the stool brown. In complete biliary obstruction, stools lose their normal color and become light gray (clay-colored stool). Some urobilinogen is reabsorbed, extracted by hepatocytes, and re-excreted in bile (enterohepatic circulation). A small amount is excreted in urine.
Because conjugated bilirubin is excreted in urine and unconjugated bilirubin is not, only conjugated hyperbilirubinemia (eg, due to hepatocellular or cholestatic jaundice) causes bilirubinuria.
Other liver functions
The liver is a complex organ involved in many biochemical processes including regulation of carbohydrate, lipid, and protein metabolism (including the storage of glucose and glycogen); control of cholesterol metabolism; and formation of key proteins including albumin, clotting factors, enzymes, and complements. The liver also functions as a filter and has a key role in purifying and removing waste products and toxins (medications, foreign substances) from the blood stream. Dysregulation of normal liver functions can manifest in clinical outcomes such as bleeding disorders, increased susceptibility to infection, derangements in blood sugar, and portal hypertensive complications such as hepatic encephalopathy from increased build up of waste products like ammonia. The liver is a complex organ involved in many biochemical processes including regulation of carbohydrate, lipid, and protein metabolism (including the storage of glucose and glycogen); control of cholesterol metabolism; and formation of key proteins including albumin, clotting factors, enzymes, and complements. The liver also functions as a filter and has a key role in purifying and removing waste products and toxins (medications, foreign substances) from the blood stream. Dysregulation of normal liver functions can manifest in clinical outcomes such as bleeding disorders, increased susceptibility to infection, derangements in blood sugar, and portal hypertensive complications such as hepatic encephalopathy from increased build up of waste products like ammonia.
Pathophysiology of Liver Disorders
Liver disorders can result from a wide variety of insults, including infections, medications, illicit substances, toxins, ischemia, and autoimmune disorders. Occasionally, liver dysfunction can occur in the postoperative setting. Most liver disorders cause some degree of hepatocellular injury and necrosis, resulting in various abnormal laboratory test results and, sometimes, symptoms. Symptoms may be due to liver disease itself (eg, jaundice due to acute hepatitis) or to complications of liver disease (eg, acute gastrointestinal bleeding due to cirrhosis and portal hypertension).
Specific diseases preferentially affect certain hepatobiliary structures or functions:
Acute viral hepatitis: Damage to hepatocytes or hepatocellular injury
Primary biliary cholangitis: Impairment of biliary secretion (cholestasis);
Cirrhosis: Liver fibrosis and resultant portal venous hypertension
The region of the hepatobiliary system affected determines the symptoms, signs, and laboratory abnormalities (see testing for hepatic and biliary disorders). Some disorders (eg, severe alcohol-related liver disease) affect multiple liver structures, resulting in a combination of patterns of symptoms, signs, and laboratory abnormalities.
After necrosis, the liver can regenerate itself. Even extensive necrosis can resolve completely (eg, in acute viral hepatitis). Incomplete regeneration and fibrosis, however, may result from injury that bridges entire lobules or from less pronounced but ongoing damage.
The prognosis of serious complications is worse in older adults, who are less able to recover from severe physiologic stresses and to tolerate toxic accumulations.
Drugs Mentioned In This Article