Herpes simplex virus infection causes recurring episodes of small, painful, fluid-filled blisters on the skin, mouth, lips (cold sores), eyes, or genitals.
This very contagious viral infection is spread by direct contact with sores or sometimes contact with an affected area when no sores are present.
Herpes causes blisters or sores in the mouth or on the genitals and, often with the first infection, a fever and general feeling of illness.
The virus sometimes infects other parts of the body, including the eyes and brain.
Usually, doctors easily recognize the sores caused by herpes, but sometimes analysis of material from a sore or blood tests are necessary.
No medication can get rid of the virus, but antiviral medications can help relieve symptoms and help symptoms resolve a little sooner.
Herpes simplex is one of several types of herpesviruses. There are two types of herpes simplex virus (HSV):
HSV-1, which is the usual cause of cold sores on the lips (herpes labialis) and sores on the cornea of the eye (herpes simplex keratitis)
HSV-2, which is the usual cause of genital herpes (although HSV-1 can also cause genital herpes)
Infection can also occur in other parts of the body such as the brain (a serious illness) or gastrointestinal tract. Widespread infection may occur in newborns or in people with a weakened immune system, particularly those who have HIV infection.
HSV is very contagious and can be spread by direct contact with sores and sometimes by contact with the mouth (oral area) or genitals of people who have HSV infection even when no sores are can be seen.
Primary and recurrent (reactivated) infection
After the first (primary) infection, HSV, like other herpesviruses, remains inactive (dormant or latent) in the body for life. A latent infection may not cause symptoms again, or it may periodically reactivate and cause symptoms.
The primary HSV infection produces an eruption of tiny blisters. After the eruption of blisters subsides, the virus remains in a dormant state inside the collection of nerve cells (ganglia) near the spinal cord that supply the nerve fibers to the infected area. Periodically, the virus reactivates, begins multiplying again, and travels through the nerve fibers back to the skin—causing eruptions of blisters in the same area of skin as the earlier infection. Sometimes the virus is present on the skin or mucous membranes even when no blisters can be seen.
The virus may reactivate many times. Reactivation of a latent oral or genital HSV infection may be triggered by the following:
A fever
Emotional stress
Suppression of the immune system (for example, by a medication taken to prevent rejection of an organ transplant)
Physical trauma, such as a dental procedure
Overexposure of the lips to sunlight
Often, the trigger is unknown.
Symptoms and Complications of HSV Infections
Tiny blisters appear on the following:
Skin: Particularly around the mouth or on the genitals
Mucous membranes: Including those lining the eyes, vagina, cervix, or inside of the mouth.
The skin around the blisters is often red.
Oral infection
The first oral infection with HSV usually causes many painful sores inside the mouth (herpetic gingivostomatitis). Herpetic gingivostomatitis most commonly develops in children.
People usually feel sick and have a fever, a headache, and body aches.
The mouth sores last 10 to 19 days and are often very severe, making eating and drinking extremely uncomfortable. As a result, people may become dehydrated. Occasionally, no symptoms develop.
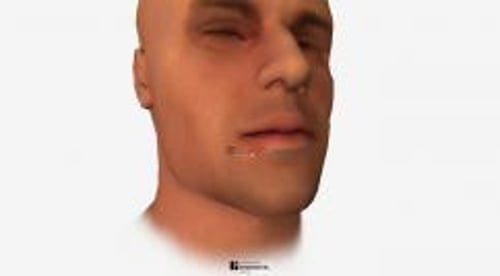
Recurrences usually produce a cluster of sores on the rim of the lip.
The lip sore is called a cold sore or fever blister (so named because they are often triggered by colds or fevers). Other triggers include over-exposure to sun on the lips, anxiety, certain dental procedures, and any condition that reduces the body's resistance to infection.
Image courtesy of Dr. Herrmann via the Public Health Image Library of the Centers for Disease Control and Prevention.
Before a cold sore appears, people usually feel a tingling at the site, lasting from minutes to a few hours, followed by redness and swelling. Usually, fluid-filled blisters form and break open, leaving sores. The sores quickly form a scab. After about 5 to 10 days, the scab falls off and the episode ends. Less often, tingling and redness occur without blister formation.
Other infections and complications
Genital herpes causes painful blisters in the genital and/or anal area. In women, internal blisters may develop in the vagina or on the cervix. Internal blisters are less painful and are not visible. The blisters develop 4 to 7 days after people are infected. The blisters go away but may come back (recur) because the virus never truly leaves the body. Blisters caused by a first genital infection are usually more painful, last longer, and are more widespread than those caused by a recurrent infection.
In people with a weakened immune system, recurrences of oral or genital herpes can result in progressive, gradually enlarging sores that take weeks to heal. The infection may progress inside the body, moving into the esophagus, lungs, or colon. Ulcers in the esophagus cause pain during swallowing, and lung infection causes pneumonia with cough and shortness of breath.
Sometimes HSV-1 or HSV-2 enters through a break in the skin of a finger, causing a swollen, painful, red fingertip (herpetic whitlow). Health care workers who are exposed to saliva or other body secretions (such as dentists) when not wearing gloves are most commonly affected.
DR P. MARAZZI/SCIENCE PHOTO LIBRARY
HSV-1 can infect the cornea of the eye. This infection (called herpes simplex keratitis) causes a painful sore, tearing, sensitivity to light, and blurred vision. Over time, particularly without treatment, the cornea can become cloudy, causing a significant loss of vision.
Infants or adults with a skin disorder called atopic eczema can develop a potentially severe HSV infection in the area of skin that has the eczema (eczema herpeticum). Therefore, people with atopic eczema should avoid being near anyone with an active herpes infection.
HSV can infect the brain. This infection (called herpes encephalitis) begins with confusion, fever, and seizures and can be fatal.
Infrequently, a pregnant woman can transmit HSV infection to her baby (called neonatal herpes). Transmission usually occurs at birth, when the baby comes into contact with infected secretions in the birth canal. Rarely, HSV is transmitted to the fetus during pregnancy. Transmission during birth is more likely when
The mother has recently acquired the herpes infection
The mother has visible herpes sores in the vaginal area, although babies may become infected from mothers who have no apparent sores
When acquired at birth, the infection appears between the first and fourth week of life. Newborns with HSV infection become very ill. They may have widespread disease, brain infection, or skin infection. Without treatment, about 85% of those with widespread disease and about half of those with a brain infection die. Even with treatment, many have brain damage.
Diagnosis of HSV Infections
Testing of a sample taken from the sore
If doctors suspect a brain infection, magnetic resonance imaging and a spinal tap
Herpes simplex virus infection is usually easy for doctors to recognize. If unsure, doctors may use a swab to take a sample of material from the sore and send the swab to a laboratory to grow (culture) and identify the virus.
Material from the sore can also be tested using polymerase chain reaction (PCR) to identify the herpes simplex DNA. PCR is a more sensitive test than viral culture, which means it will miss fewer cases of the virus.
Sometimes doctors examine material scraped from the blisters under a microscope. Although the virus itself cannot be seen, scrapings sometimes contain enlarged infected cells (giant cells) that are characteristic of infection by a herpes-type virus.
Blood tests to identify antibodies to HSV can also be helpful. (Antibodies are produced by the immune system to help defend the body against a particular attacker, such as HSV.)
Certain blood tests can distinguish between HSV-1 infection and HSV-2 infection.
If a brain infection is suspected, magnetic resonance imaging (MRI) of the brain and a spinal tap (lumbar puncture) to obtain a sample of cerebrospinal fluid for analysis may be done.
Treatment of HSV Infections
Antiviral medications
No current antiviral treatments can eradicate HSV infection, and treatment of a first oral or genital infection does not prevent chronic infection of nerves. However, during recurrences, antiviral medications such as acyclovir, valacyclovir, or famciclovir, may relieve discomfort slightly and help symptoms resolve a day or two sooner (see table No current antiviral treatments can eradicate HSV infection, and treatment of a first oral or genital infection does not prevent chronic infection of nerves. However, during recurrences, antiviral medications such as acyclovir, valacyclovir, or famciclovir, may relieve discomfort slightly and help symptoms resolve a day or two sooner (see tableSome Antiviral Medications for Herpesvirus Infections). Treatment is most effective if started early, usually within a few hours after symptoms start—preferably at the first sign of tingling or discomfort, before blisters appear. For people who have frequent, painful attacks, the number of outbreaks can be reduced by taking antivirals every day indefinitely (called suppressive therapy). However, taking antivirals does not necessarily prevent infected people from transmitting the infection. Most antivirals are available by prescription only.
Penciclovir cream, applied every 2 hours during waking hours, can shorten the healing time and duration of symptoms of a cold sore by about a day. Nonprescription creams containing docosanol (applied 5 times a day) may provide some relief. Acyclovir, valacyclovir, or famciclovir taken by mouth for up to a few days may be the most effective treatment for recurring cold sores.Penciclovir cream, applied every 2 hours during waking hours, can shorten the healing time and duration of symptoms of a cold sore by about a day. Nonprescription creams containing docosanol (applied 5 times a day) may provide some relief. Acyclovir, valacyclovir, or famciclovir taken by mouth for up to a few days may be the most effective treatment for recurring cold sores.
Severe HSV infections, including herpes encephalitis and infections in newborns, are treated with acyclovir given intravenously. If the virus becomes resistant to acyclovir, which is very rare, foscarnet can be given intravenously., are treated with acyclovir given intravenously. If the virus becomes resistant to acyclovir, which is very rare, foscarnet can be given intravenously.
People with herpes simplex keratitis may be given trifluridine eye drops. An ophthalmologist should supervise treatment.may be given trifluridine eye drops. An ophthalmologist should supervise treatment.
Other treatments
For people who have minimal discomfort, the only treatment needed for recurring herpes of the lips or genitals is to keep the infected area clean such as by gentle washing with soap and water. Applying ice may be soothing and reduce swelling.
Applying prescription or nonprescription topical anesthetics, such as benzocaine, may help relieve pain. If the mouth contains many sores, the mouth can be rinsed with lidocaine. These anesthetics should not be swallowed. Topical anesthetics should only be taken as directed. If taken more often than directed, these medications can have harmful side effects.Applying prescription or nonprescription topical anesthetics, such as benzocaine, may help relieve pain. If the mouth contains many sores, the mouth can be rinsed with lidocaine. These anesthetics should not be swallowed. Topical anesthetics should only be taken as directed. If taken more often than directed, these medications can have harmful side effects.
Pain relievers may be taken for pain.
Prevention of HSV Infections
People with HSV infection should avoid activities and other things known to trigger recurrences. For example, people with oral HSV infection triggered by sunlight should avoid exposure to sunlight as much as possible or use sunscreen when sunlight cannot be avoided.
Because HSV infection is contagious, people with infection of the lips should avoid kissing as soon as they feel the first tingling (or, if no tingling is felt, when a blister appears) until the sore has completely healed. They should not share a drinking glass and, if possible, should not touch their lips. They should also avoid oral sex.
People with genital herpes should use condoms at all times. Even when there are no visible blisters and no symptoms, the virus may be present on the genitals and can be spread to sex partners.
Drugs Mentioned In This Article